Latest Advancements in US Nanotechnology for Medical Applications
Significant advancements in US-based nanotechnology are revolutionizing medical applications, from targeted drug delivery and enhanced diagnostics to regenerative medicine and advanced bioimaging, promising transformative impacts on patient care and disease treatment.
The convergence of science and engineering has ushered in an era where the smallest scales yield the biggest potential. For those in the medical field or simply curious about future healthcare, understanding What are the Latest Advancements in US-Based Nanotechnology for Medical Applications? is critical. This dynamic field is rapidly reshaping how we diagnose, treat, and even prevent diseases.
The Dawn of Nanomedicine: A New Frontier in Healthcare
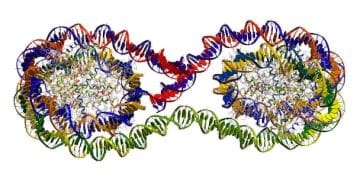
Nanotechnology, the manipulation of matter on an atomic, molecular, and supramolecular scale, typically ranging from 1 to 100 nanometers, has profound implications for medicine. This field, often termed nanomedicine, is transforming traditional medical approaches by enabling unprecedented precision and efficiency in diagnostics, therapeutics, and regenerative medicine. The United States has emerged as a global leader in this innovative space, driven by substantial research investments and collaborative efforts between academia, industry, and government agencies.
The inherent advantages of working at the nanoscale are numerous. Materials at this size exhibit unique physical, chemical, and biological properties compared to their bulk counterparts. For instance, nanoparticles can exhibit enhanced reactivity, increased surface area-to-volume ratio, and novel optical properties. These characteristics are precisely what drug developers, diagnosticians, and bioengineers are leveraging to overcome long-standing challenges in healthcare.
Enhanced Precision in Drug Delivery
One of the most immediate and impactful applications of nanomedicine is in drug delivery. Traditional chemotherapy, for example, often affects healthy cells along with cancerous ones, leading to severe side effects. Nanotechnology offers a solution by enabling targeted drug delivery, where therapeutic agents are encapsulated within nanoparticles designed to specifically seek out diseased cells or tissues.
- • Liposomal Nanoparticles: Widely adopted, these lipid-based vesicles encapsulate drugs, protecting them from degradation and allowing for controlled release at target sites.
- • Polymer Nanoparticles: Biodegradable polymers can be engineered to carry various therapeutic payloads, offering tunable release profiles and surface modification for specific targeting.
- • Dendrimers: Highly branched, synthetic macromolecules that offer precise control over size, shape, and surface chemistry, making them ideal for drug entrapment and targeted delivery.
This precision not only minimizes collateral damage to healthy tissues but also often allows for lower overall drug dosages, reducing systemic toxicity and improving patient outcomes. The ability to concentrate therapeutics directly at the site of action is a game-changer for conditions ranging from cancer to infectious diseases.
Beyond active targeting, where nanoparticles are functionalized to bind to specific disease markers, passive targeting also plays a significant role. This often relies on the enhanced permeability and retention (EPR) effect, commonly observed in tumor tissues, where leaky vasculature allows nanoparticles to accumulate preferentially within the tumor microenvironment.
The ongoing research in this area continues to refine these systems, exploring new materials, trigger-responsive release mechanisms (e.g., pH, temperature, light), and combination therapies. The goal remains to create smarter, more efficient drug delivery systems that can navigate the complex biological landscape of the human body with unparalleled accuracy.
Revolutionizing Diagnostics: Early Detection and Advanced Imaging
The ability to detect diseases early and image biological processes with high resolution is paramount in effective medical intervention. Nanotechnology is providing unprecedented tools that push the boundaries of conventional diagnostics and imaging techniques. This means earlier diagnoses, better monitoring of disease progression, and more precise guidance for surgical procedures.
Advanced Bioimaging Techniques
Nanoparticles act as superior contrast agents and imaging probes, offering enhanced signal-to-noise ratios and the capacity for multi-modal imaging. Traditional imaging methods, such as MRI or CT scans, can often benefit from these nanoscale enhancements.
- • Quantum Dots (QDs): Semiconductor nanocrystals that emit light when excited, offering highly stable and bright fluorescence for imaging live cells and tissues with exceptional clarity. Their tunable emission spectra allow for multiplexed imaging.
- • Gold Nanoparticles: These can scatter and absorb light very efficiently, making them excellent contrast agents for optical imaging, and they also have applications in photoacoustic imaging due to their strong light absorption.
- • Magnetic Nanoparticles: Superparamagnetic iron oxide nanoparticles (SPIONs) are used as MRI contrast agents, providing improved resolution and the ability to detect specific cellular and molecular targets.
These novel imaging agents enable clinicians and researchers to visualize biological structures and processes at a much finer scale, facilitating the detection of minute tumors, tracking immune cell movements, or analyzing protein interactions within cells. The enhanced sensitivity means that pathological changes can be identified even before macroscopic symptoms appear.
Beyond imaging, nanotechnology is making strides in point-of-care diagnostics. For instance, nanosensors are being developed that can detect biomarkers of disease in minute quantities of blood, urine, or saliva, potentially allowing for rapid and accurate diagnoses outside of traditional laboratory settings. This decentralization of diagnostics could be particularly transformative for rural areas or developing countries where access to sophisticated medical facilities is limited.
Innovations in nano-enabled diagnostic platforms also include lab-on-a-chip devices and microfluidic systems that can perform complex analyses using tiny sample volumes. These systems integrate multiple laboratory functions onto a single chip, increasing speed, reducing costs, and improving diagnostic accuracy. The ongoing development in this area promises a future where personalized and highly sensitive diagnostic tests are readily available.
Regenerative Medicine and Tissue Engineering
The field of regenerative medicine seeks to repair, replace, or regenerate damaged tissues and organs. Here, nanotechnology is playing an increasingly vital role, particularly in scaffolding, cell-material interactions, and controlled release of growth factors. Building materials at the nanoscale allows for the creation of environments that closely mimic the body’s natural cellular architecture.
Nanomaterials can be engineered to guide cell growth, differentiation, and tissue formation. For example, electrospun nanofiber scaffolds provide a three-dimensional environment that closely resembles the extracellular matrix, offering physical cues that direct cell behavior. These scaffolds are being explored for applications ranging from bone regeneration to nerve repair and skin grafting.
Biocompatible Nanomaterials for Tissue Repair
The choice of material is crucial in regenerative medicine, requiring strict biocompatibility and often biodegradability. Nanomaterials offer these properties along with the unique ability to interact at the cellular level.
- • Nanofiber Scaffolds: Created from polymers or ceramics, these provide structural support and a surface for cell attachment, proliferation, and differentiation, mimicking natural tissue structures.
- • Nanohydrogels: Water-rich polymer networks with nanoscale features that can encapsulate cells and biomolecules, providing a soft, hydrated environment conducive to tissue growth.
- • Carbon Nanotubes & Graphene: These carbon-based nanomaterials exhibit exceptional mechanical strength and electrical conductivity, making them promising for nerve regeneration and cardiac tissue engineering.
Furthermore, nanotechnology facilitates the controlled release of growth factors, cytokines, and other bioactive molecules essential for tissue regeneration. Nanoparticles can encapsulate these delicate therapeutic agents, protecting them until they are needed at the site of injury, ensuring their sustained and localized delivery. This level of control is virtually impossible with traditional bulk materials.
The interface between nanomaterials and biological systems is complex, and research continues to delve into how these materials influence cell behavior at a fundamental level. Understanding these interactions is key to designing more effective regenerative therapies. For instance, surface modifications of nanoparticles can be tailored to promote specific cell responses, such as osteogenesis (bone formation) or angiogenesis (blood vessel formation).
The ultimate goal is to create functional, living tissues and organs for transplantation, reducing dependence on organ donation and improving the quality of life for patients with chronic diseases or injuries. While still in its early stages for many complex applications, the promise of nanoregenerative medicine is immense, with ongoing clinical trials for specific applications showing encouraging results.
Addressing Global Health Challenges: Infection and Prevention
Infectious diseases remain a significant global health threat, often complicated by antimicrobial resistance and the emergence of new pathogens. Nanotechnology offers innovative solutions for combating these challenges, from novel antimicrobial agents to advanced vaccine delivery systems.
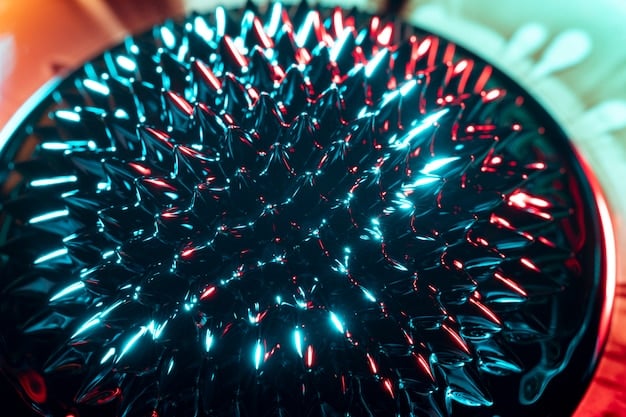
Traditional antibiotics are becoming less effective against increasingly resistant bacteria. Nanomaterials provide a new arsenal. Silver nanoparticles, for example, have long been known for their antimicrobial properties and are being integrated into wound dressings and medical devices to prevent infections. Other metal nanoparticles, such as copper and zinc oxide, are also being explored for their broad-spectrum antimicrobial activity.
Nanomaterials in Antimicrobial Strategies
The unique properties of nanoparticles, such as high surface area and the ability to penetrate bacterial cell walls, make them potent antimicrobial agents. They can also overcome resistance mechanisms that thwart traditional antibiotics.
- • Metal Nanoparticles: Silver, copper, and titanium dioxide nanoparticles demonstrate broad-spectrum antimicrobial activity by damaging bacterial cell membranes, producing reactive oxygen species, and inhibiting enzyme function.
- • Antimicrobial Peptides & Enzymes on Nanocarriers: Encapsulating or conjugating these natural antimicrobials with nanoparticles can enhance their stability, targeting, and efficacy, while reducing systemic toxicity.
- • Photothermal/Photodynamic Nanotherapeutics: Nanomaterials that convert light into heat or produce reactive oxygen species when exposed to light can selectively destroy pathogens while minimizing harm to surrounding healthy tissues.
Beyond direct antimicrobial action, nanotechnology is critical in developing advanced vaccine platforms. Nanoparticle-based vaccines can present antigens to the immune system more effectively, eliciting stronger and more prolonged immune responses. This is particularly relevant for difficult-to-target pathogens or rapidly mutating viruses.
For instance, lipid nanoparticles (LNPs) have become a cornerstone in mRNA vaccine technology, as demonstrated by their pivotal role in COVID-19 vaccines. LNPs protect the mRNA molecules from degradation, facilitate their delivery into host cells, and induce an effective immune response. This success highlights the transformative potential of nanocarriers for future vaccine development against a wide array of infectious diseases.
Furthermore, nanosensors capable of rapid detection of pathogens can provide early warning systems for outbreaks, helping to contain the spread of disease more effectively. The integration of nanotechnology into public health strategies promises a future with more robust defenses against microbial threats and more efficient outbreak management.
Biosensors and Nanorobotics: The Future of Intervention
The concept of “smart” medicine, where diagnosis and treatment are performed by microscopic agents within the body, is moving from science fiction to reality, thanks to the advancements in biosensors and nanorobotics. These technologies promise unprecedented levels of precision and autonomy in medical interventions.
Biosensors integrated with nanomaterials offer superior sensitivity and specificity for detecting biological molecules. A biosensor typically consists of a biological recognition element (e.g., an antibody, enzyme, or DNA strand) coupled with a transducer that converts the biological signal into a measurable electrical or optical signal. Nanomaterials enhance this transduction process significantly.
Cutting-Edge Biosensor Development
The integration of nanomaterials into biosensors yields devices with enhanced performance, capable of detecting extremely low concentrations of analytes, crucial for early disease diagnosis and monitoring.
- • Nanowire and Nanotube Sensors: The high surface-to-volume ratio of these materials makes them highly sensitive to molecular binding events, enabling ultra-low detection limits for biomarkers.
- • Plasmonic Nanosensors: Utilize the unique optical properties of metallic nanoparticles (e.g., gold or silver) to detect molecular interactions based on changes in their surface plasmon resonance.
- • Lab-on-a-Chip Devices with Nanosensors: Miniaturized systems that integrate multiple analytical steps on a single chip, utilizing nanosensors for rapid and comprehensive biochemical analysis, often at the point of care.
Nanorobotics, while still largely in the research phase, represents the ultimate frontier in nanomedicine. Imagine microscopic robots, programmed to navigate the bloodstream, identify cancer cells, deliver drugs precisely, or even perform delicate microsurgeries within the body. While fully autonomous nanorobots are years away, significant progress is being made in developing rudimentary forms.
For example, micro- and nanomotors, propelled by chemical reactions or external magnetic fields, are being developed to transport drug payloads or move through biological fluids. These early prototypes lay the groundwork for future applications such as targeted tumor ablation, clearing arterial blockages, or delivering gene therapies to specific cells.
The ethical implications and regulatory challenges for such advanced technologies are vast and are being actively discussed. However, the potential to perform non-invasive, highly precise medical procedures using nanorobots is a compelling vision that continues to drive research and innovation in this fascinating field.
Challenges and Ethical Considerations in Nanomedicine
Despite the immense promise, the path from laboratory breakthroughs to widespread clinical adoption in nanomedicine is fraught with challenges. These include technical hurdles, regulatory complexities, and crucial ethical considerations that demand careful attention.
One of the primary technical challenges is the large-scale manufacturing of uniform and stable nanomaterials. Reproducibility and consistency are critical for clinical applications, yet controlling nanoparticle size, shape, and surface chemistry on an industrial scale remains difficult. Furthermore, understanding the long-term pharmacokinetics and pharmacodynamics of nanoparticles in the human body is essential. How do they distribute, metabolize, and excrete? What are their potential long-term toxicities?
Navigating the Roadblocks to Clinical Translation
Translating cutting-edge nanomedicine research into marketable, safe, and effective clinical products requires overcoming significant scientific, regulatory, and economic hurdles.
- • Toxicity and Biocompatibility: Ensuring that nanoparticles are safe for long-term use in the human body without causing adverse immune reactions or accumulating in vital organs.
- • Manufacturing Scalability: Developing cost-effective and reproducible methods for synthesizing nanoparticles at a scale sufficient for clinical and commercial demands.
- • Regulatory Frameworks: Establishing clear and robust guidelines for the approval of nanomedicine products, balancing innovation with patient safety, unique from traditional drugs or devices.
The regulatory pathway for nanomedicine products is often ambiguous, as they frequently straddle the lines between drugs, devices, and biologics. Regulatory bodies like the FDA in the US are continually working to adapt their frameworks to assess the safety and efficacy of these novel products. This involves developing new testing paradigms and risk assessment strategies specific to nanoscale materials.
Ethical considerations are equally important. Issues surrounding patient privacy with highly detailed diagnostic data, the potential for genetic manipulation via gene delivery using nanoparticles, and equitable access to these potentially high-cost therapies are all critical. Ensuring that the benefits of nanomedicine are accessible to all, not just a privileged few, is a significant societal challenge.
Moreover, public perception and education play a vital role. Addressing concerns about “nanoparticles in the body” with transparency and clear, evidence-based communication is essential to foster trust and acceptance. Responsible development and deployment of nanomedicine require a multi-stakeholder approach involving scientists, clinicians, ethicists, policymakers, and the public.
Despite these challenges, the trajectory of nanomedicine is overwhelmingly positive. Continued interdisciplinary research, robust regulatory science, and open ethical dialogue will be crucial in realizing the full potential of this transformative field, ensuring that its benefits are safely and equitably brought to patients worldwide.

The Horizon of Nanomedicine: What Comes Next?
The journey of nanotechnology in medical applications is still in its early to middle stages, with a vast horizon of possibilities yet to be explored. The advancements witnessed so far are merely a prelude to even more sophisticated and integrated systems that will redefine healthcare.
One key trend is the increasing convergence of nanomedicine with artificial intelligence (AI) and machine learning (ML). AI can analyze vast datasets from nanoparticle formulations, biological interactions, and clinical outcomes, accelerating the discovery and optimization of new nanotherapeutics. ML algorithms can predict nanoparticle behavior in complex biological systems, reducing the need for extensive trial-and-error experimentation.
Emerging Trends and Future Directions
The future of nanomedicine is likely to involve more integrated, intelligent, and personalized approaches, leveraging synergistic technologies for unprecedented therapeutic outcomes.
- • “Smart” Nanodevices: Development of nanoparticles with integrated sensing, computing, and actuation capabilities, capable of performing complex diagnostic and therapeutic tasks autonomously within the body.
- • Personalized Nanomedicine: Tailoring nanoparticle-based therapies to an individual’s unique genetic makeup, disease profile, and physiological responses for maximal efficacy and minimal side effects.
- • Nano-enabled Gene Editing: Utilizing nanoparticles for precise and efficient delivery of gene-editing tools (e.g., CRISPR-Cas9) to specific cells, opening new avenues for treating genetic disorders.
The concept of “theranostics,” which combines therapeutic and diagnostic capabilities within a single nanoparticle system, is gaining significant traction. This allows for real-time monitoring of drug delivery and treatment efficacy, enabling clinicians to adjust therapies dynamically for optimal patient outcomes. Imagine a nanoparticle that can image a tumor, release a drug, and then report back on the tumor’s response—all in one go.
Another exciting area is the development of in situ nanofabrication, where nanoscale structures are assembled directly within the body. While highly complex, this could lead to the formation of localized drug reservoirs or even microscopic implants that repair damaged tissues over extended periods. Such advancements would require sophisticated control over molecular self-assembly and biological interactions.
Furthermore, research into biocompatible and biodegradable materials for nanomedicine will continue to evolve, seeking to minimize any long-term retention or toxicity issues. The development of “stealth” nanoparticles that can evade the body’s immune system for longer circulation times will also be crucial for enhancing therapeutic delivery.
Ultimately, the future of nanomedicine is about creating highly efficient, targeted, and minimally invasive solutions to complex medical problems. It promises a shift from broad-spectrum treatments to highly personalized and precise interventions, fundamentally improving disease management and patient well-being across a vast spectrum of conditions. The ongoing research and investment in the US are pivotal in realizing this transformative future.
| Key Area | Brief Advancement |
|---|---|
| 💊 Targeted Drug Delivery | Nanoparticles precisely deliver drugs to disease sites, enhancing efficacy and reducing side effects. |
| 🔬 Advanced Diagnostics | Nanosensors and contrast agents enable earlier and more precise disease detection and imaging. |
| 🩹 Regenerative Medicine | Nanofiber scaffolds and hydrogels guide tissue growth and repair, mimicking natural bodily structures. |
| 🛡️ Infection Control & Vax | Nanoparticles offer novel antimicrobials and enhanced vaccine delivery platforms. |
Frequently Asked Questions About Nanomedicine
▼
Nanomedicine is the application of nanotechnology to healthcare, involving the use of materials engineered at the nanoscale (1-100 nanometers). Unlike traditional medicine, which often operates at the macro or micro scale, nanomedicine leverages the unique properties of nanoscale materials to enable more precise diagnostics, targeted drug delivery, and intricate tissue engineering, offering unprecedented control at the cellular and molecular levels.
▼
For cancer treatment, nanoparticles are designed to encapsulate chemotherapy drugs, protecting them from degradation and enabling targeted delivery. They can passively accumulate in tumors due to leaky blood vessels (EPR effect) or be actively engineered to bind to specific markers on cancer cells. This precision minimizes damage to healthy cells, reduces side effects, and increases drug concentration at the tumor site, improving therapeutic outcomes.
▼
Nanotechnology significantly enhances medical imaging by providing superior contrast agents and imaging probes. Nanoparticles like quantum dots, gold nanoparticles, and magnetic nanoparticles offer improved resolution, increased signal-to-noise ratios, and the ability to detect specific molecular targets. This allows for earlier diagnosis of diseases, precise visualization of tissues, and real-time monitoring of biological processes, surpassing the capabilities of conventional imaging methods.
▼
Yes, ethical concerns exist. These include potential long-term toxicity of nanoparticles, implications for patient privacy with highly detailed diagnostic data, the responsible use of gene-editing technologies delivered via nanoparticles, and ensuring equitable access to potentially high-cost nanomedicine therapies. Open dialogue among scientists, ethicists, policymakers, and the public is vital to address these challenges responsibly and ensure broad benefit.
▼
While largely in research, nanorobotics holds immense promise for future medical applications. Prospects include microscopic robots navigating the body to perform highly targeted drug delivery, precise microsurgeries, clearing arterial blockages, or even delivering gene therapies to specific cells. Early prototypes of micro- and nanomotors are already being developed, laying the groundwork for increasingly autonomous and precise in-vivo interventions.
Conclusion
The landscape of medical science is undergoing a profound transformation, largely driven by the relentless pace of innovation in US-based nanotechnology. From the extraordinary precision offered by targeted drug delivery systems to the enhanced capabilities of diagnostic imaging and the foundational role in regenerative medicine, nanomedicine is not merely an incremental improvement but a paradigm shift. While challenges related to safety, regulation, and ethical considerations persist, ongoing research and collaborative efforts across academia, industry, and government are systematically addressing these hurdles. The future promises even more sophisticated integration of nanotechnology with fields like AI, paving the way for personalized, highly effective, and minimally invasive healthcare solutions that could reshape our approach to health and disease management for generations to come.